A Reflection on My Placement
A Reflection on My Placement
Introduction
The purpose of this essay is to review how nursing has improved my individual and skilful life in my opening year in the nursing’s program. My discussion entails my experiences with the five crucial skills shapes, which entail care, fluid management, teamwork, compassion, communication, medication management, and nutrition. To demonstrate an understanding of the five skills, I will apply a recognised model of reflection. Reflection is a technique used to learn from past incidents and make healthcare deliveries safer. This essay will follow The Gibbs reflective cycle model (O’Carroll and Park 2007) as it provides a chance for structuring the discussion.
Gibbs Reflective Cycle
According to Gibbs, there are six steps to completing one cycle that can help me continuously better my nursing practice as well as take lessons from experiences to do better in the future (O’Carroll and Park 2007). As part of the cycle, a description of the situation is presented, followed by an analysis of emotions, then a final evaluation, a fourth stage, contains an analysis of the occurrence. Thereby, there is whatever else that could have been done is in the conclusion, which is in the fifth stage, and the closing stage is the plan of action that is used to prepare for the condition in the future.
Gibbs Reflective Pictorial Representation
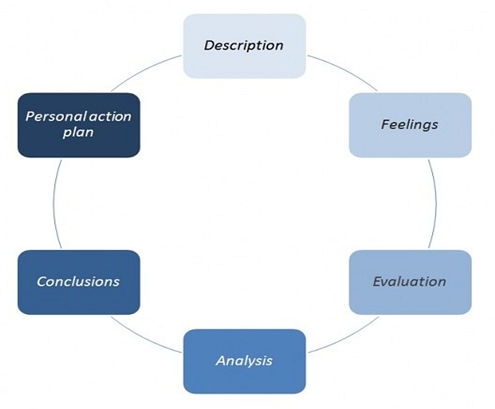
(Reflective model according to Gibbs 2022)
- Description
It is important to note that all confidential information relating to patients, wards, hospitals and professional colleagues has not been included in this paper to ensure ethical practice and adherence to the NMC code of professional conduct, section 5 which affirms that I must guard against breaches of confidentiality' (NMC 2008). My placement areas were both general paediatric wards, which both included inpatient beds for children, and a day unit for surgical and paediatric patients. Health care services are provided within a children's ward for children between the ages of one and seventeen. Children's wards specialise in providing health care to infants through teenagers. Nursing is an important component of promoting healthy behaviour, and children's nurses are no exception (Moules and Ramsey 1998).
Nurturing a child requires far more than caring for a miniature adult. It involves understanding the process through which a healthy child grows into adulthood. Furthermore, it also involves learning how to minimise the effect of child illness or hospitalisation. Ideally, this includes partnering with either the parents or people who look after the child at home.
Additionally, communication is a complicating factor in treating the younger child. Being adults, we can express how we feel or identify the intensity and nature of pain in our bodies. In contrast, children may not be able to communicate as clearly, and thus, our nurses have to interpret their behaviours and reactions correctly. As such, it is crucial for nurses to be capable of noticing the health of a child is deteriorating rapidly as children can develop illnesses at any time (Toso et al., 2016, pp.182-191).
- Feelings
The role I played within the clinical setting and the relationships I had with others were important to me. To establish a mutual understanding and trust with other team members, I felt it was vital for me to build the team member relationship. Based on my reflections about my strengths and weaknesses, in terms of my role and relationships with others, I believe that whilst I have nearly fully grasped my role as a nurse in caring for paediatric patients. However, I feel that I lack a substantial understanding of the roles of the other healthcare professionals with whom I work in the care of these same patients. As a collaborative healthcare team member, my priority has been given a medium to high rating since I feel that it is impossible to be successful without an understanding of the roles of the other team members I work with. When other healthcare professionals are not well understood, it is difficult for me to understand why they should be involved in the care of my patients, or even when it is appropriate to include other healthcare professionals, ultimately lowering the quality of the patient's care. Therefore, I decided to interact more with others during my two placements to work alongside them with confidence and help them achieve the same goals as I did.
- Evaluation
A child's health can affect his or her development, and hence, it is important to work with the family or caregiver to make that the child does not endure additional stress while hospitalised or ill. When I began working in this ward, I was both excited and apprehensive. I was excited as this would be a new experience and the chance to learn more about diseases and conditions, but I was apprehensive as to how illnesses impact individuals and their families, as well as the challenges they might encounter and the ways they would respond. My lack of experience and knowledge about illnesses was a potential weakness for me, and thus, I needed to have a clear understanding of my strength and weakness before I begin working as Nurse. The ability to interact effectively with patients requires awareness of one's capabilities as well. Individual beliefs and opinions can have either a positive or negative impact on how we view other individuals.
Maintaining non-judgmental behaviour requires an understanding of strengths and weaknesses, as well as the capacity to reflect on individual characteristics. A nurse must put the care of the individual first by making sure they are treated as an individual and their dignity respected (Andrews et al., 2010, pp.251-255). As a clinician, I am aware that it is important to give attention to the patient rather than the behaviour. I learned about the various kinds of patients we would meet throughout my nursing program, including their different health diagnoses, as well as patients’ individual rehabilitation and their recovery plans, which gave me an insight into the needs of patients and how illness can affect an individual. Furthermore, it gave me more confidence to approach each patient with individual individualised attention and to begin to build nurse-patient relationships after my mentor gave this information. A relationship between a nurse and a patient goes through three phases: orientation, working, and termination (Wolf et al., 1998, Pg. 99).
- Analysis
Most people, me included, are firm believers that first impressions make lasting impressions; thus, I make sure I do my best to introduce myself to others in a professional manner. To establish the nurse-patient relationship, I sought to establish a rapport when introducing myself to the patient. It is essential that one must present him/herself as a compassionate, warm, and caring person to enable building trust and respect between the nurse and the patient, which is a key component of showing caring to others. The need for care and compassion is a natural and informal skill used in communication, and it plays an important role in social exchange (Baughan and Smith 2013). According to Ratnasari et al. (2019) five qualities constitute caring, and these five qualities are termed "the 5 C's". Among them, are commitment (providing the necessary care for every patient), compassion (sharing in how others feel) and empathy (the ability to understand the feelings of another person). Other than that, a nurse should have the competence to apply nursing processes through problem solving and decision-making. Additionally, patients' trust can be achieved through the nurse having confidence in themselves, and them being confident in the nurse. Lastly, the nurse should have a conscience and have an ethical conviction, as well as act in accordance with the standards of the nursing profession.
As part of my placement, I have been able to observe multidisciplinary team meetings and participate in meetings with healthcare professionals, such as physiotherapists, as well as participate in ward rounds with doctors and nurses during the time on placement. The team on the ward where I was placed was excellent. I always felt like I was part of the team, and that I made a valuable contribution since I was always ready to take on whatever they threw at me, and because they were inclusive and supportive. I noticed that it is not a good idea to hold back and wait for people to notice you. Thereby, one should not be afraid to show their interest every day, and new opportunities will present themselves.
In order to establish strong relationships with the patients, I had to spend quality time with each patient. This enabled me to build strong relations founded on honesty, trust, and respect. The most important thing to me is that each patient has the confidence that I can help meet their individual needs and trust me to provide them with the best care and support available. Caring for and showing compassion to patients requires the ability to empathise with them and relate to their emotions. Empathy is rooted in the ability to relate to others, understand their feelings, and sense their meanings (Walker and Alligood, 2001, pp.140-147). By understanding patients' perspectives, one can engage in interactions that offer more support, motivation and engagement, which I wished to show the patients in the wards of that unit. In addition to further developing my communication skills, which I learned from my earliest clinical placement, I was eager to spend time with each patient and get to know them through my inpatient placement since this would help me hone my nursing skills further.
A nurse's ability to effectively communicate with her or his patient is an essential component necessary for one to be a better nurse (Slade et al. 2015). Consequently, it is crucial to have good communication skills. According to Riley (2015), the two-way process of communication is complicated; it entails people conveying messages using both verbal and non-verbal means. For the patient to feel comfortable and be able to speak freely, showing genuine interest and concern is essential. In the course of communication, the tone and habit 'paralinguistic' applied, as well as how the individual perceives these, may enhance or inhibit the development of the relationship. Self-esteem and identity can be damaged by a comment made (Pennington 2012). My communication skills are one of my interpersonal strengths, and I found comfort in communicating with patients. However, I felt a little cautious sometimes, for instance, when asked a question to which I did not have a clear answer.
In order to remain objective in my conversations with patients, I observed how health professionals communicated before engaging in meaningful conversations with patients. Initial interactions and communication with each individual varied. The degree of interaction and communication reflected the age of the patient and their parents, as well as how they were capable of trusting me despite my being a student. For effective communication, active listening is a necessary skill. In this way, important information will be obtained regarding the patient's wishes and concerns through non-verbal communication. Providing the correct information will also allow time to provide an appropriate response and insight into the care required. To acknowledge a general interest in what is being discussed, it is equally significant to demonstrate active listening through maintaining eye contact, proper facial expressions, and nods. Furthermore, it is important to be observant of the patient’s body language and listen to their speech for one to know when they are uncomfortable and when they are experiencing cognitive deficits.
With respect to patient care, I wanted to demonstrate that I listened carefully to each patient, and that I was truly interested in what they had to say and to gain their trust so they could express their opinions and feelings to me on the basis of confidence and mutual respect. It was important that I demonstrated care, compassion, and communication skills for a therapeutic relationship to be developed with all the patients. Having a healthy mutual relationship will benefit the patient in terms of meeting their holistic needs, as well as the nurse gathering the pertinent information to provide suitable intercession (McQueen, 2004, pp.101-108).
During this placement, I had been exceptionally eager to gain knowledge and skills related to medication management. A well-managed medicine supply chain ensures that patients receive the maximum benefit from their prescribed medicines while minimising any reactions (Evans and Day 2005). My first placement provided me with the opportunity to administer medication to patients under supervision, which meant I was acquainted with administering medication correctly according to the NMC medication guidelines (Andrews et al., 2010, pp.251-255). The first placement helped me gain confidence in my ability to safely administer medications to patients, and the second placement helped me demonstrate safe practices as soon as I started.
Before administering any medication to a patient, I knew I needed to follow the eight important rights of medication, which include the right to treat the right patient, to have proper medicine, to keep time, to know the date of medication, to be prescribed the right dose, to use the right route, to preparation by the doctor or nurse, and the right to have the right documentation. In light of the accountability nurses face when managing medications, I wanted to ensure I was competent during this placement by learning as much as possible. I also wanted to become familiar with the legislation that underpins medication management, including the Medicines Act (1968) and the Misuse of Drugs Act (1971) (“Drug Laws”). In accordance with the NMC guidelines and Trust policy, all medication administrations must be accurately recorded.
The importance of nutrition and hydration is essential to maintaining good health, and poor nutrition can often complicate childhood diseases. Patient B is being treated with insulin injections twice a day for type 1 diabetes. A diabetic person develops diabetes when the pancreas is unable to produce insulin, which is the hormone that causes sugars within the bloodstream to accumulate (Taylor, 2008, pp.1781-1789). Patient B is considered obese because of his body mass index, which is 27. Patients B and C suffer from urinary tract infections (UTIs). Patient B underwent a nutritional assessment when he was admitted to the ward in October based on guidelines established by the National Institute for Health and Clinical Excellence (NICE).
- Conclusion
I gained a lot of knowledge on assessing and formulating a care plan during my two long placements. Particularly, I learnt that in order to create a proper care plan one needed to assess the current risks as well as those that may come in the future. Depending on how it is defined, a risk represents a negative event or an adverse consequence that could be harmful. All medical records relating to Patient B needed to be accurate and an evidence approach needed to be applied to reduce risk. After obtaining the patient’s information from his nutritional assessment tools and care documents, I created an intervention and plan of care according to the risks discovered. There were two major areas of risk for Patient B's parents: he was not following a healthy diet and was not consuming enough fluids.
In addition, I administered an intramuscular (IM) cytotoxic injection to Patient A during my placement. Applying infection control, prevention, and prevention procedures were imperative during the administration process. Prevention of infection and control procedures are designed to break the infection chain and decrease the risk of infection for both staff and patients. I was approached by my mentor and was asked to hold the child. At first, I was afraid of the process as there seemed to be so many precautions to take, but after making several observations and understanding the procedure, it became easier for me. In the process, it was necessary to adhere to hand hygiene, such as washing my hands before starting the procedure, wearing protective gear like pair of gloves, the safe use and disposal of sharp objects, and aprons. Using aprons and gloves that were in good condition and disposing the used needle into a cytotoxic sharps container were the steps I followed. As soon as I had completed the procedure, I discarded all PPE and all items containing the patient’s bodily fluids.
- Personal Action Plan
A plan of action was identified to monitor Patient B's nutritional needs, including using a food and fluid intake chart daily, as well as a food menu chart on a weekly basis to record detailed information about his diet and fluid intake. Weekly weight measurement was also necessary for Patient B. As part of the intervention plan, a poor diet and inadequate fluid intake were identified as factors contributing to Patient B's decrease in health. The task of monitoring Patient B's daily diet and fluid intake, as well as maintaining accurate documentation and continuity of care, became an integral part of my everyday routine while on shift. This revealed to me a unique perspective on the significance of accuracy in the continuity of care and documentation. Keeping good records is important for ensuring the safety and effectiveness of care (Standards for Medicines Management). By observing the food and fluid intake of patient B, it certainly was obvious that he was finding it difficult to maintain a regular diet on his own. His intake of fluid was also declining, which affected both his diabetes and his physical well-being.
After reflecting on my experiences in my previous placements, I think I would follow that specific course. The experience I gained from my first placement has helped me continue to develop my skills and enhance my knowledge. In this essay, I have shown my preparedness to gain knowledge and skills, as well as reveal a professional attitude in the entire placement setting. Throughout, I have grown more knowledgeable and confident in the five crucial shapes of care, demonstrating my willingness to learn. My experience gaining knowledge and skills has been highly positive, and I now feel confident in my abilities as a nurse. However, I would modify some areas for future placements based on my experiences in the past. Researching more about the specific client group and setting would help me prepare better for challenges encountered in the paediatric care setting.
Summary
To summarize, I believe having this training would have benefitted me greatly during my subsequent placement since I noticed I was not fully prepared when administering the first injection, and how the effects may differ between different patients. I felt unsure of how to communicate with some patients during my first week on placement, and felt like more preparation would have enabled me to communicate well with the patients as well as build their confidence and help them relax. All in all, the experience has been beneficial since I gained a good understanding of how to develop and maintain good nursing skills that are crucial in areas such as medication management, care organisation, infection prevention and control, communication, nutrition, as well as better communication.
Reference
Andrews, M., Brewer, M., Buchan, T., Denne, A., Hammond, J., Hardy, G., Jacobs, L., McKenzie, L. and West, S., 2010. Implementation and sustainability of the nursing and midwifery standards for mentoring in the UK. Nurse Education in Practice, 10(5), pp.251-255.
Baughan, J. and Smith, A., 2013. Compassion, caring and communication: skills for nursing practice. Routledge.
Evans, S.J. and Day, S.J., 2005. Medicines and Healthcare Products Regulatory Agency (MHRA)(Formerly MCA). Encyclopedia of Biostatistics, 5.
Moules, T. and Ramsay, J., 1998. The textbook of children's nursing. Nelson Thorne McQueen, A.C., 2004. Emotional intelligence in nursing work. Journal of advanced nursing, 47(1), pp.101-108. “National Institute for Health and Care Excellence.” GOV.UK, https://www.nice.org.uk/ Nursing and Midwifery Code of Professional Conduct. London: Nursing Council (2008) and Midwifery Council.
O'Carroll, M. and Park, A., 2007. Essential mental health nursing skills. Elsevier Health Sciences. Pennington, D.C., 2012. Social cognition. Routledge.
Ratnasari, R.T., Gunawan, S., Anshori, M., Ryandono, M.N.H. and Herianingrum, S., 2019. Anteseden and Consequences of Health Performance Based on Patient intimacy. Opcion, 35(S22), pp.526-548.
Riley, J.B., 2015. Communication in nursing. Elsevier Health Sciences.
Slade, D., Manidis, M., McGregor, J., Scheeres, H., Chandler, E., Stein-Parbury, J., Dunston, R., Herke, M. and Matthiessen, C.M., 2015. Communicating in hospital emergency departments. Springer.
Taylor, R., 2008. Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia, 51(10), pp.1781-1789.
Toso, B.R.G.D.O., Filippon, J. and Giovanella, L., 2016. Nurses' performance on primary care in the National Health Service in England. Revista Brasileira de Enfermagem, 69, pp.182-191.
Walker, K.M. and Alligood, M.R., 2001. Empathy from a nursing perspective: Moving beyond borrowed theory. Archives of Psychiatric Nursing, 15(3), pp.140-147. Wolf, Z.R.,
Colahan, M., Costello, A. and Warwick, F., 1998. Relationship between nurse caring and patient satisfaction. Medsurg Nursing, 7(2), p.99.